
Excessive menstrual bleeding (menorrhagia), is a debilitating condition that affects approximately 22% of all menstruating women and accounts for more than 30% of the 600,000 hysterectomies performed in the United States. Hysterectomy, the second most frequently performed surgical procedure in the United States, is the most common surgical treatment for menorrhagia. Although hysterectomy provides a cure for menorrhagia, it is often accompanied by numerous physical and psychological effects. Hysterectomies performed to treat excessive menstrual bleeding cost the U.S. healthcare system an estimated $1.5 billion annually.
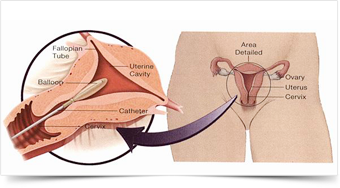
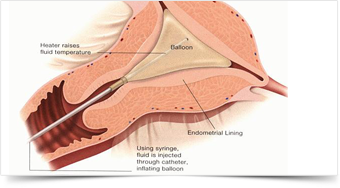
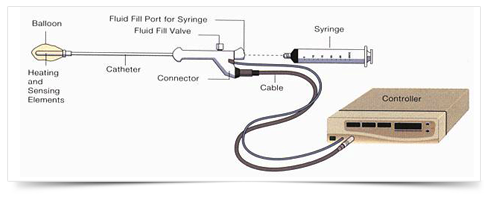
It is a new outpatient procedure to reduce excessive menstrual bleeding. Unlike hysterectomy, which takes out the entire uterus, the procedure just destroys the lining of the uterus by the use of heat.
In most cases, bleeding during your period will be reduced to moderate or light flow. Some women may experience spotting; a few may experience no bleeding at all. Clinical data has shown that up to 15% of patients may not respond to ThermaChoice therapy and may require additional treatment.
Your doctor must rule out abnormal uterine conditions like some fibroids, and your pap smear and biopsy must also be normal. This is not a treatment for uterine cancer. If you will want to have children, ThermaChoice is not an option since the uterine lining is destroyed during therapy.
First, a soft, flexible balloon attached to a thin catheter (tube) is inserted into the vagina, through the cervix and placed gently into the uterus.
This therapy should not be used if you ever want to have children - in fact, pregnancies after ablation can be dangerous for both fetus and mother. Since there is a chance pregnancy could occur, contraception or sterilization should be used after treatment. Please discuss these options with your physician.
About an hour before therapy, your physician may give you medication which minimizes cramping during and after the procedure. You may also be given a mild sedative to help you relax. In most cases, you will be awake during the procedure and may experience cramping and/or discomfort. Your doctor may use a local anesthesia to numb the cervix and the uterus. Sometimes patients want to be "put to sleep" using general anesthesia after which you may experience some nausea. This is an option for you to discuss with your doctor.
You may feel mild or moderate cramping like a menstrual period, and if needed, your doctor will give you a mild medication to make you feel more comfortable. After 1-4 hours in the recovery room, you should arrange to be driven home where you can take it easy for the rest of the day.
Most women can return to work and family commitments by the next day. Sexual activity can be resumed after your first check-up, usually 7-10 days. Most patients have a pinkish and watery discharge for about 2 weeks, sometimes as long as a month. In most cases, the first few periods after the procedure may continue to be heavy but will begin to improve thereafter.
You should call your physician if you develop a fever of 100.4° F or over, worsening pelvic pain that is not relieved by ibuprofen (Motrin or Advil) or other medication prescribed by your physician, nausea, vomiting, bowel or bladder problems, and/or a greenish vaginal discharge.
The procedure may pose some rare, but possible, safety risks including blood loss, heat burn of internal organs, electrical burn, perforation (hole) or rupture of the wall of the uterus, or leakage of heated fluid from the balloon into the cervix or vagina. Collection of blood or tissue in the uterus and/or fallopian tubes during the months post-procedure is also possible and may require an outpatient procedure to correct the problem.
As with any type of uterine procedure, there may also be the risk of infection, usually easily managed with oral antibiotic therapy.
Caution: This product contains natural latex rubber which may cause allergic reactions.
Enter your details below & we will call you back