
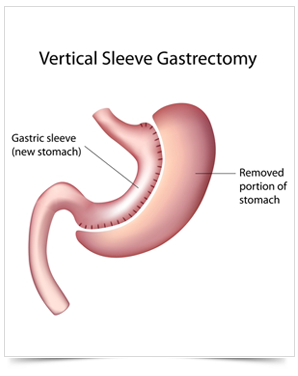
The laparoscopic sleeve gastrectomy is a bariatric procedure in which the surgeon removes approximately 85% of the stomach, shaping the remaining stomach into a tube or “sleeve”. It can be used as a first stage operation prior to a gastric bypass or as a definite procedure.
During the laparoscopic gastric sleeve the nerves of the stomach and the outlet valve (pylorus) are not altered, preserving the function of the stomach. Other advantages:
In the laparoscopic sleeve gastrectomy the stomach is divided along its vertical length in order to create a slender pouch. The excess stomach is removed. The purpose is to limit the amount of food ingested at any give time (restrictive operation), without altering the normal absorption of the vitamins and minerals.
Sleeve gastrectomy is a restrictive procedure. It greatly reduces the size of the stomach and limits the amount of food that can be eaten at one time. It does not cause decreased absorption of nutrients or bypass the intestines. After this surgery, patients feel full after eating very small amounts of food. Sleeve gastrectomy may also cause a decrease in appetite. In addition to reducing the size of the stomach, the procedure reduces the amount of the “hunger hormone,” ghrelin, produced by the stomach.
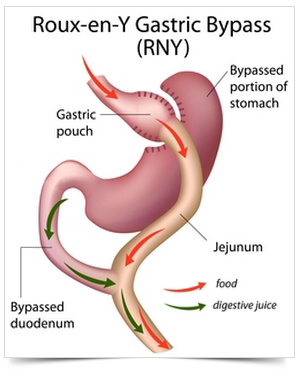
Gastric bypass surgery makes the stomach smaller and causes food to bypass part of the small intestine. You will feel full more quickly than when your stomach was its original size. This reduces the amount of food you can eat at one time. Bypassing part of the intestine reduces how much food and nutrients are absorbed. This leads to weight loss.
One type of gastric bypass surgery is a Roux-en-Y gastric bypass.
In normal digestion, food passes through the stomach and enters the small intestine, where most of the nutrients and calories are absorbed. It then passes into the large intestine (colon), and the remaining waste is eventually excreted.
In a Roux-en-Y gastric bypass ,only a small part of the stomach is used to create a new stomach pouch, roughly the size of an egg. The smaller stomach is connected directly to the middle portion of the small intestine (jejunum), bypassing the rest of the stomach and the upper portion of the small intestine (duodenum).
This procedure is done by making several small incisions and using small instruments and a camera to guide the surgery (laparoscopic approach).
Risks common to all surgeries for weight loss include an infection in the incision, a leak from the stomach into the abdominal cavity or where the intestine is connected (resulting in an infection called peritonitis), and a blood clot in the legs (deep vein thrombosis, or DVT) or lung (pulmonary embolism). Some people develop gallstones or a nutritional deficiency condition such as anemia or osteoporosis.
Other risks from Roux-en-Y gastric bypass include:
Our Medical Weight Loss Program with involves a thorough initial medical and lifestyle consultation with specific plans for long term planning and follow up. Programs include either individual or group nutritional and behavioral instruction related to eating problems, metabolic testing, review of individual medical conditions which either cause or are affected by weight and the development of individual exercise prescriptions. We specialize in developing programs for long term weight loss management. The strategy is to incorporate individual weight history, genetic background, social situations and current stressors along with extensive traditional evaluations of medications, and concurrent medical concerns into a chronic disease approach.
Every month there are new individual issues. Every day there are new eating challenges and the potential for novel insight and interventions. The tools of weight management are changing. Current medical treatment of excess weight and weight-related diseases utilizes many treatment options including, but not limited to: medications, behavioral life strategy tools, nutritional education, meal planning, meal replacements, and of course, exercise. No strategy works in a vacuum. No strategy works forever and that is why diets do not work. Food choices and life stressors affect us many times a day. Every person has a unique story. Yet sometimes patients gain understanding and commitment from groups. Everyone is different and everyone deserves their own chronic disease care program.
Medical Weight Loss options:
Many medical conditions worsen with increasing weight. Some are metabolic diseases like diabetes and some are mobility diseases as knee pain and osteoarthritis. The understanding and treatment of weight and coexisting diseases goes hand in hand.
Hunger can be distracting and defeating. Medications can often help us gain control of our hunger and urges while we concurrently put other lifestyle strategies into place. Medications are a tool and work best when used as part of a comprehensive weight management plan.
Many medications used to treat common diseases as hypertension, diabetes, depression, seizures and arthritic conditions can contribute to weight gain. There may be alternative medications or ways to ameliorate the disease processes so as to utilize less medicine in general.
One can be severely overweight and malnourished due to an overuse of carbohydrates, and fast foods. Patients who have had a weight loss surgery or for any other reason have taken in too few calories and vitamins or vomited frequently are also at risk of malnutrition. Fatigue, achiness, balance problems or confusion may be due to a weight related vitamin deficiency or a protein deficiency.
Research shows that pre-packaged nutritionally balanced low calorie food choices help to maintain weight loss and can be a mainstay of weight loss success. Over the counter or special medically supervised meal replacement products are used depending on individual patient needs. We helps each individual patient figure out which meal replacement strategy might suit him or her at any one time.
Planning ahead makes it easier to deal with the stressors of the day without sacrificing the benefits of well-balanced diet. Meal planning as well as food logs may be used to improve self- accountability as well as nutritional awareness.
This is a cornerstone of all individual and/or group curriculums. Changing how one eats, understanding one’s eating cues and understanding head hunger vs. metabolic needs is key. It is important to learn how to manage inevitable stress and life-changing events without over-eating or cutting back on activity. We all need to practice and fine tune these skills to develop a kind and safe individual strategy.
Part of mindful eating is to learn to read labels, menus and general food composition while setting into motion how to utilize this knowledge into one’s busy life style and one’s family preferences as well. Holiday and special events can be a barrier to weight loss and weight management, so planning is important.
When do you need to weight yourself? How much of a diet history must you do? How many labels should you read? How do you know you are “safe”? There are many strategies. What works for one person may not work for another. But we do know that staying accountable to yourself helps weight loss and prevents weight regain. This should be done in the spirit of curiosity and not guilt or dread.
Diabetics, patients with insulin resistance, women with PCOS (polycystic ovarian syndrome), or with a history of gestational diabetes have unique vulnerabilities related to glucose (sugar) metabolism. Our team works intensively with you to develop safe low calorie and very low carbohydrate meal plans which often seem to jump start and accelerate weight loss while maintaining glucose control.
Walking may be painful and even damage joint surfaces when there is extra weight to bear. There are many considerations on how to find a safe, comfortable, easy to do exercise program: sitting, water, reclining, pacing, frequency.
factors can be addressed to find safe exercise? What about strength training? Who needs a stress test? What about supportive shoes? Do I need a trainer? How do I find a gym? I hate gyms, so what do I do? How do I use a gym? Why do I need to exercise anyway? Research shows that people who exercise doing something they love and especially if it is with someone they enjoy, these people are resistant to weight regain.
Practice and repetition. Overweight issues are a chronic disease process which reflect societal, genetic and individual vulnerability that usually needs to be addressed for the rest of one’s life. Life hits us sideways and issues crop up. Sometimes we may need different tools: surgery, medication, VLCD meal plans, group talking, or specialty referrals to many therapists (orthopedists, cardiologists, psychologists to name a few). If you have a Weight & Wellness Specialist which you see routinely (usually ever 4 weeks), new life issues, new insights and new medical concerns are addressed and strategies and instituted. This is the best obesity care possible for any disease. And you deserve it. There is hope when you know that there are solutions as long as you keep coming. It is not simple but you are not alone.
Enter your details below & we will call you back